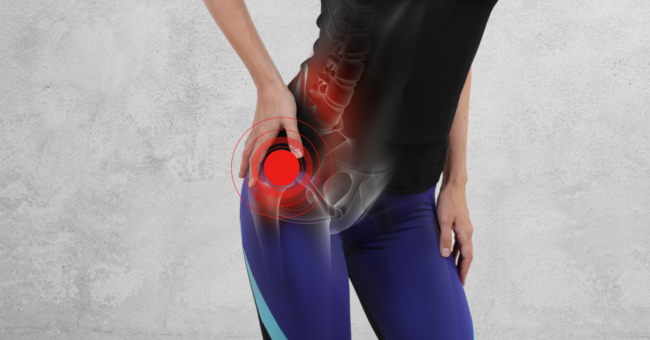
Hip bursitis
What is hip bursitis?
Hip bursitis is a common pathology in physiotherapy offices that is often accompanied by other associated symptoms that reduce the quality of life.
First of all, we will define what bursae are: they are serous or synovial bags found in various parts of the body (hips, shoulder, heels or knee) and whose main function is to act as “shock absorbers” for anatomical areas of special stress or mechanical conflict, thus avoiding excessive friction.

When referring to hip bursitis we can refer to several different ones:
- When we speak of those located around the greater trochanter (trochanteric bursitis) whose function is to allow the gluteus maximus tendon to slide with the tensor fascia lata muscle as it passes through the greater trochanter (lateral bony projection of the femur).
- The one located in the iliac psoas muscle, located in the internal part of the joint and whose pain is manifested in the inguinal region.
Of the two, trochanteric bursitis is the most common and therefore we will focus on it to provide information on the pathology as well as possible solutions from the field of physiotherapy.
Symptoms of trochanteric bursitis
The most common symptoms in trochanteric bursitis are:
- Pain: It is usually the most common symptom. In a first phase it is a sharp stabbing pain in the trochanter (extending towards the external region of the thigh), progressively it becomes a diffuse pain that can cover the entire area of the hip joint and buttocks.
It usually increases after sitting for long periods of time and getting up, after walking long distances and when going up or down stairs. It makes it difficult to rest, since it is painful to sleep leaning on that side.
- Inflammation. Perceptible to palpation.
- Warmth in the area or redness.
- Functional limitation of the hip joint. sensation of stiffness.
Causes of hip bursitis
The most common causes for the appearance of hip bursitis are usually repeated movements of the joint (sometimes accompanied by poor joint dynamics or neuromuscular imbalance) or sustained positions in which excessive and prolonged pressure is exerted on the bursa.
Other causes may be:
- Trauma to the area.
- Rheumatoid arthritis.
- Infections (commonly bacterial).
- Spinal disorders (scoliosis)
- Diabetes
- Inflammatory systemic pathologies.
Risk factors of hip bursitis
Anyone is susceptible to hip bursitis in their lifetime, however there are risk factors that can increase the risk:
- Age: older age usually increases the risk.
- Professions or sports activities: sports such as running, or professions such as dancing.
- Inadequate footwear.
- Weight.
- Muscle dysfunction in the lumbar or hip region: poor recruitment of the muscles responsible for this area can lead to excessive friction on the bursa in the medium term, triggering symptoms without previous trauma.
Treatments
From physiotherapy we can provide multiple solutions for both symptom reduction and total recovery.
Conventional physiotherapy
Conventional physiotherapy has several tools such as ultrasound, magnetotherapy, laser, manual therapy of the musculature that inserts into the trochanter, electrotherapy (TENS, interferential), cryotherapy, etc.
Advanced physiotherapy
From advanced physiotherapy, however, we can obtain better results and with a greater speed in the response of the tissues to the therapy:
- INDIBA – Tecartherapy: Advanced physiotherapy technique in which by means of radiofrequency (non-invasive) we achieve an effect of biostimulation, vascularization and hyperactivation and thus achieve better oxygenation of tissues, drainage of toxins and activate the body’s own mechanisms for cell regeneration.
- EPI (Percutaneous Intratisular Electrolysis): Technique consisting of applying a stimulus to the tissues by means of galvanic current through a needle that we position in the target tissue by means of ultrasound control.
- Echoguided Percutaneous Neuromodulation: by means of needles similar to those of acupuncture we apply a low frequency current to the nerves in charge of both the sensitivity of the area and the motor control of the musculature involved in its movement. In this way we can achieve both an improvement in muscle work (reducing the chances of relapse) and a considerable decrease in pain.
Medical therapies
We must also take into account the possible medical therapies that can help such as nerve block or infiltration with corticosteroids in the bursa decreasing inflammation in the same in just hours noticing a significant decrease in pain.
It should be noted that none of these techniques or therapies are incompatible with the others, indeed, the good choice of one or the other depending on the degree of injury and the particularities of the patient is what sometimes marks the success of the treatment.
In our MIVI centers we have a team specialized in both the assessment and the treatments described above in order to resolve any questions that may arise regarding this ailment and to choose the therapy with the greatest possibilities of therapeutic benefit.