Everything you need to know about spinal cord stimulator therapy
A bit of history
The idea of using electrical current to relieve pain is not new. In the 1960s, researchers discovered that by electrically stimulating certain areas of the nervous system, pain perception could be altered. This principle led to the first human implantable spinal cord stimulation systems in 1967.
Since then, the technology has evolved enormously. Today, spinal cord stimulators are sophisticated, minimally invasive and highly customizable devices used in leading hospitals around the world.
What is spinal cord neurostimulation?
Spinal neurostimulation involves sending small electrical impulses to the spinal cord, a key structure of the nervous system that transmits signals between the body and the brain. These impulses act by “jamming” or modulating pain signals before they reach the brain.
The device that generates these impulses is implanted in the patient’s body and acts in a continuous or programmed manner, without producing systemic side effects such as those that can occur with drugs.
Where are the electrodes placed?
The electrodes are placed in the epidural space, which is an anatomical area located just outside the spinal cord and inside the spinal canal. The nerve roots that carry sensory and motor signals pass through this space.
The precise placement of the electrodes in the appropriate area of the spine (usually at the thoracic or lumbar level) is key to achieving a good result. It is performed under radiological control and usually with local anesthesia and sedation.
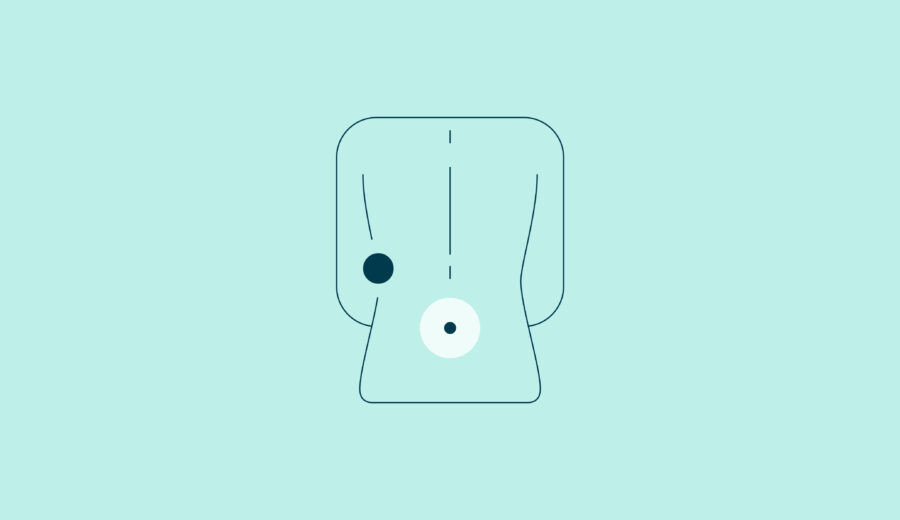
What is the device like?
A spinal cord stimulation system consists of three components:
1. Stimulation electrodes or leads: these are introduced into the epidural space through a small incision and connected to the generator.
Generator or battery: it is usually implanted under the skin, in the abdominal or buttock area. It can be rechargeable or non-rechargeable.
3. External controller: the patient uses it to turn the stimulation on or off, adjust the intensity or switch between preset programs.
For whom is this therapy indicated?
Neurostimulation is recommended for patients with chronic neuropathic pain that has not responded to other treatments. Some of the most frequent indications are:
– Failed spinal surgery syndrome (FBSS)
– Chronic radiculopathies (such as persistent sciatica after surgery)
– Complex regional pain syndrome (CRPS)
– Refractory ischemic pain
– Phantom limb pain
– Chronic perineal or abdominal pain neuropathic
Before definitive implantation, a temporary test phase (lasting a few days) is performed, in which the electrodes are placed and an external generator is connected to check for significant pain relief.
What can be expected from the treatment?
Studies show that a significant proportion of patients achieve a pain reduction of at least 50%, which translates into:
– Reduced consumption of analgesics (including opioids)
– Better night’s rest
– Increased functional capacity and physical activity
– Improved mood and reduced anxiety/depression
However, not all patients respond in the same way, which is why the testing phase is essential to assess the efficacy in each individual case.
What are the risks and possible complications?
Although it is a safe and minimally invasive technique, like any medical procedure, it can have risks:
Immediate surgical risks:
– Infection at the implant site (sometimes requiring removal of the device)
– Bruising or bleeding
– Pain at the incision site
Late complications:
– Electrode migration: can cause loss of efficacy if the electrode moves out of place.
– “Painful pocket”: occurs when the generator causes discomfort or pressure in the area where it is housed.
– Generator failure or deterioration of the wiring.
– Need for replacement: in non-rechargeable generators, replacements are usually required every 3-5 years. Rechargeable generators can last more than 10 years.
Technological innovations: what’s new?
Recent years have brought significant improvements:
– Smaller devices: ultra-compact and discreet generators that fit better on the body.
– Long battery life: up to 10-15 years in rechargeable models. Some do not need daily recharging, but weekly or even less.
– Stimulation without paresthesia: new modalities that do not produce a tingling sensation (high frequency waves, bursts…).
– Compatibility with magnetic resonance imaging (MRI): many current models allow MRI under certain conditions, which is highly valued.
– Mobile control: apps that allow patients to easily adjust their therapy.
What if it doesn’t work in the future?
One of the advantages of neurostimulation is that it is reversible. If it is no longer useful, if a serious complication appears, or if the patient wishes, the device can be removed without permanent sequelae.
In addition, it is possible to adjust the stimulation programs over time, or even change the generator while maintaining the electrodes if they are still in good condition.
In a nutshell
Spinal neurostimulation represents a breakthrough in the treatment of resistant chronic pain. It does not eliminate the cause of the pain, but it can modify the way the body perceives it, significantly improving quality of life.
If you are considering this option or it has been suggested to you by your medical team, at MIVI we will help you assess whether it is right for you. The approach is always individualized and multidisciplinary, looking for the treatment to suit your needs and goals.
Dr. Isaac Peña