Fibromyalgia: the invisible pain that has an explanation
Fibromyalgia remains one of the most difficult to diagnose and, at the same time, one of the most misunderstood diseases. It mainly affects women and usually takes years to be identified. We spoke with Dr. Jorge Orduña to clarify the keys to diagnosis, debunk myths and explore effective treatment options to improve patients’ quality of life.
Why is fibromyalgia so difficult to diagnose?
Unlike other diseases, fibromyalgia does not show up in blood tests or imaging tests. This can be frustrating for both patients and healthcare professionals. Diagnosis is based on clinical criteria, medical experience and ruling out other causes of
Common myths: more harm than help
One of the most common misconceptions is that fibromyalgia “does not exist” or that it is “only psychological”. Although emotional factors may play a role, this does not negate the fact that there is a clear neurophysiological basis. People with fibromyalgia have increased sensitivity to pain due to alterations in sensory processing. Another harmful myth is that patients exaggerate. In reality, the pain is real, constant and widespread.
What happens when the patient is not believed?
The lack of medical and social credibility generates profound consequences: anxiety, sadness, isolation and a worsening of the general condition. Validating the patient, listening to his or her story and providing clear information has a real and positive therapeutic impact.
Is there a common profile among fibromyalgia sufferers?
There is no “fibromyalgic personality” as such, but there are shared traits in many patients: self-demanding, responsible, emotionally sensitive individuals who have lived through prolonged stressful situations. These traits do not cause the disease, but they can influence its evolution and how pain is coped with.
Labor impact: a little visible reality
Fibromyalgia directly affects occupational performance. Chronic pain, fatigue and cognitive difficulties can lead to absenteeism or even loss of employment. Therefore, it is necessary to talk about work adaptations, flexible schedules and the official recognition of this condition as a cause of partial disability.
New therapeutic approaches: there is hope
Although there is currently no definitive cure, there are effective tools to improve quality of life. Some of the emerging treatments that are showing good results include:
-
Personalized and adapted physical exercise
-
Mindfulness techniques and stress management
-
Psychotherapy with a focus on chronic pain
-
Education in pain neuroscience
-
Multidisciplinary approaches
-
Neurostimulation in selected cases
The approach must be individualized and person-centered, with an integrated view of the person’s physical, emotional and social situation.
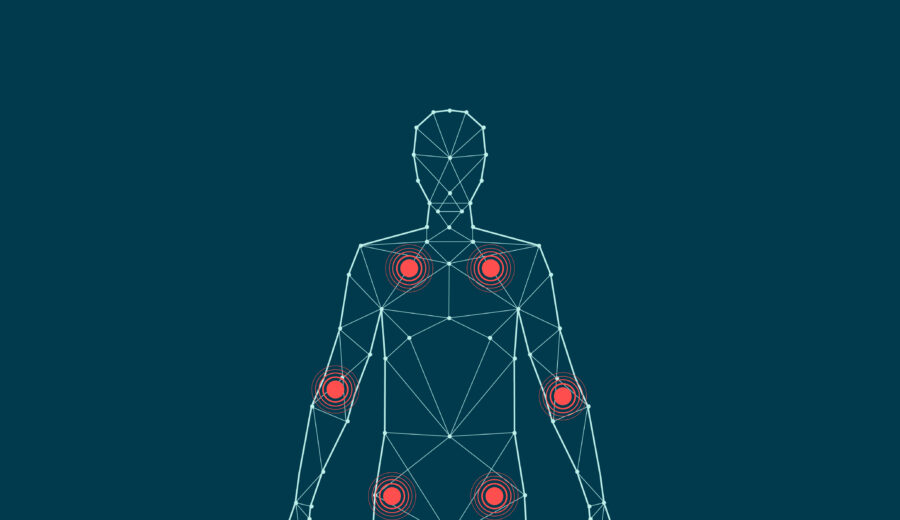
Central sensitization: the neurological key to pain
People with fibromyalgia present a phenomenon known as central sensitization, in which the nervous system amplifies normal signals, interpreting them as painful. This explains why pain is perceived without visible lesions: the origin lies in how the brain and spinal cord process sensory information.
Stress as a trigger
Although not the sole cause, sustained stress is a factor that can act as a trigger in predisposed individuals. Sleep disturbances, emotional trauma or mental overload may contribute to activate this state of hypersensitivity.
Underdiagnosis: a worrisome situation in Spain
In our country, many people remain undiagnosed, often after years of medical pilgrimage. This is due to several factors: scarce specific training on chronic pain, overload in primary care, lack of specialized units and a fragmented view of the patient’s symptoms.
A message for those who have just received the diagnosis
Dr. Orduña sums it up in a sentence that may mark the beginning of a new stage:
“Your pain is real, you are not alone and there are ways to get better.”
Seeking reliable information, staying active within one’s means and surrounding oneself with specifically trained professionals can make a big difference in prognosis and well-being.

Member No.: 46-3203399
Centers:
Dr. Jorge Orduña Valls is a specialist in Anesthesiology, Resuscitation and Pain Management, and serves as National Medical Director of MIVI Salud, in addition to being Director of the Pain Unit at its headquarters in Valencia.
- He has more than ten years of experience in reference units both nationally and internationally.
- Among his training highlights: Doctoral thesis with Cum Laude mention in 2020 (University of Santiago de Compostela) , European Diploma in Pain Medicine (EDPM) awarded by European Pain Federation (EFIC) in 2017.
- He completed training stays in the USA (e.g. at the Millennium Pain Center in Bloomington, Illinois) and at centers in Miami, Germany and France.
- He is an expert in interventional techniques for pain: radiofrequency, rhizolysis, nerve blocks, etc.
- In research, he has published relevant papers, for example the study “The Nerve to Vastus Medialis as a Target for Treating Chronic Medial Knee Joint Pain: An Ultrasound-Based Anatomical Localization Study” in the journal Pain Medicine (2025) together with other specialists in the field.